Low Vision

Image source: faculty.washington.edu/chudler/armd.html
What? Low vision, sometimes known as visual impairment, is something I volunteered to write a blog post about. As a primary care physician, I confess my interests often paralleled the stage of life I was in.
Now as I am entering a more “senior” stage of life, you guessed it; the conditions or diseases which affect my age group have my attention.
Low Vision/Age-related Macular Degeneration Awareness Month is observed annually throughout February. It is an awareness month targeted at spreading more information about Age-related macular degeneration (AMD) and diseases affecting the eyes that could lead to visual impairment.
What are the numbers?
The best estimate is that there are 196 million people worldwide with AMD. It seems that those over the age of 50 are the most susceptible. In fact, AMD is the No. 1 cause of vision loss for those over age 50. There are two “types” of AMD, but we will get to that in a moment. Thirteen percent of people over the age of 85 have the condition. It is more common in people of white European ancestry and women are affected more than men. It is the leading cause of visual impairment and vision loss in developed countries.
What are the symptoms?
The most common are:
- Things look blurry at the center of something.
- It is increasingly difficult to read or do other fine tasks in low light.
- You tend to see straight lines as wavy.
- There may be blank spots in your central visual field.
- The symptoms are different depending on what type of AMD you have:
- People with dry AMD (85-90%)lose their vision slowly. They might notice a problem with one or both eyes when reading or driving. Or they might realize that they now need bright lights or a magnifying glass to see as well as they used to. People with dry AMD sometimes also notice spots that seem blurry.
- People with wet AMD (10-15%)can have sudden changes in vision. When they first notice symptoms, they might have problems in only one eye. (Later, both eyes usually develop problems.) When people with wet AMD look at straight lines, the lines look bent or wavy.
- This condition has been linked to frequent falls or injuries.
If you are worried and think you may have AMD
- Your initial evaluation will include questions about objects appearing to have distorted shapes, decreased vision, flashing light or floaters in the vision, a blind spot, and difficulty adapting to darkness. You will be asked about past eye issues; family history of eye diseases; drug history, including aspirin and antioxidant use; and social history, including smoking history.
- You should undergo a comprehensive eye examination by an ophthalmologist.
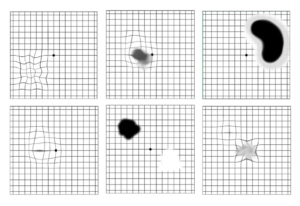
- If you have early AMD, it is likely you may be advised to self-monitor your vision with a an Amsler grid (see below for normal and abnormal examples).
- If you smoke…STOP! Smoking is the strongest modifiable risk factor. High blood pressure and high lipids have also been associated with AMD. There is, however, no evidence that the use of “statins” (cholesterol-lowering medication) has an impact.
- Other factors to consider include increasing foods rich in omega-3. These include nuts, fish like tuna, salmon, mackerel, or others.
- Consistent use of eye protection in high light situations. (Keep your sunglasses handy!)
- An increasing amount of evidence suggests that individuals with AMD are also at risk of systemic diseases such as stroke. Your primary care doctor will want to monitor your total health status.
Treatment
There is no treatment available for dry, or non-neovascular, AMD. Patients with dry AMD should be given support; advised about lifestyle modification, smoking cessation, and antioxidant supplementation; and monitored regularly.
Age-Related Eye Disease Study (AREDS) found that high-dose oral antioxidant vitamin (i.e., vitamins C and E, beta carotene) and zinc supplementation decreased progression of intermediate or advanced AMD by approximately 25%. Thus, evidence supports the use of antioxidant vitamin and mineral supplements that support ocular function, such as those studied in AREDS, to delay vision loss in patients with AMD.
Vitamin E, beta carotene, vitamin C, and multivitamin supplements have not been shown to prevent or delay AMD development.
Patients with wet, or neovascular, AMD should be referred to an ophthalmologist for management. First-line therapy is an anti-VEGF drug. This is a medicine which is an anti-growth factor for blood vessels. This drug is administered by injection directly into the eye monthly or every three months. These drugs selectively destroy blood vessels growing abnormally at the back of the eye. This can lead to improved vision for patients with neovascular AMD. There are people who start out with dry macular degeneration and then develop the wet type.
Finally
Vision rehabilitation (often called vision rehab) is a term used meaning rehabilitation to improve vision when there is low vision. In other words, it is the process of restoring functional ability and improving quality of life and independence in an individual who has lost visual function through illness or injury. The focus is on those impairments which cannot benefit from eyeglasses, contact lens, medication, or surgery. The focus is on helping people perform everyday activities. Vision rehab has been found to be extraordinarily helpful in helping people maintain their independence.
Resources
en.wikipedia.org/wiki/Vision_rehabilitation
Cheung CMG, Wong TY. Is age-related macular degeneration a manifestation of systemic disease? New prospects for early intervention and treatment. J Intern Med. 2014;276(2):140-153