Medicaid Matters
Dedicated to providing facts and information about Health First Colorado (Colorado’s Medicaid program)
Real Medicaid Facts
enrolled in Health First Colorado (Colorado’s Medicaid program)
of adults in Colorado on Medicaid are working
of births in Colorado are covered by Medicaid
of people receiving nursing home care are covered through Medicaid
Passage of OBBBA and What it Means for Health First Colorado
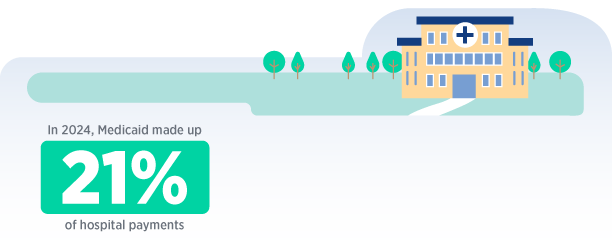
Medicaid is a vital source of health coverage, a key workforce and economic driver, and a critical piece of the safety net that supports all Colorado communities.
On July 4, 2025, President Donald Trump signed The One Big Beautiful Bill Act (OBBBA) into law. The OBBBA, also referred to as the new federal health care law, increases federal spending on border security, defense, and energy. To offset these expenses, the new law includes a $1 trillion reduction in federal health care spending over the next decade, primarily targeting Medicaid.
The new law enacts the largest Medicaid cut in U.S. history and significantly reshapes the health care landscape. Over the next decade, 10 million people across the country are expected to become uninsured as the result of the new law, and Colorado is expected to lose at least $10 billion in federal funding. Changes in the new law will require fundamental shifts to Colorado’s Medicaid program structure, operations, and financing, which will impact members, providers, and communities. Those changes will be phased in over time, and we will update this page as they take effect.

Colorado Access is Committed to Protecting Health Care Access
The new federal law represents a serious setback for the health of Coloradans and communities across the country. It brings harmful changes to programs that support people with low incomes and complex needs — programs that are essential to their well-being.
Fortunately, Colorado is represented by leaders who recognize the critical role of Medicaid. Colorado Access is proud to be part of a strong, mission-driven network of advocates and partners working to protect access to affordable, person-centered care. We will advocate for state lawmakers to move forward with care and use every available flexibility to preserve continuity of coverage and services. We stand ready to partner with them as they navigate the challenging policy landscape ahead.
At Colorado Access, our mission remains unchanged: to improve access to high-quality, affordable health care. As the federal landscape shifts, we are committed to working with partners to implement new federal requirements in ways that minimize harm and keep people at the center.
OBBBA Questions & Answers for Members
There are no immediate changes to Medicaid coverage or eligibility. Most Medicaid members are unlikely to experience significant changes or disruptions in care until late 2026. Most members will remain eligible, but there may be additional requests for information and other paperwork requirements in the future.
Colorado Access is committed to communicating broadly and transparently in advance of changes to program eligibility requirements, processes, benefits, or coverage.
The new law makes several changes that impact members directly:
- Starting October 2026, some lawfully present immigrants will no longer qualify for Medicaid including refugees, asylees, parolees, certain survivors of domestic violence or other abuse, and certain victims of human trafficking.
- The Department of Health Care Policy and Financing (HCPF) estimates this will impact roughly 7,000 current members.
- Starting in January 2027, some Medicaid members above a certain income level will be required to renew their benefits every six months, rather than every 12.
- HCPF estimates this will impact roughly 377,000 current members, but about 75% of renewals will be made automatically based on information on file or through third-party sources without the need for member engagement.
- Starting January 2027, some Medicaid members will have to show they are working, doing community service, enrolled in school, or participating in other qualifying programs for a minimum number of hours per month to qualify for benefits. Certain populations will be exempt from this requirement. The state may request federal approval to delay this requirement until as late as January 2029.
- HCPF estimates this will impact roughly 377,000 current members, though many will be exempt from meeting the community engagement requirement due to disability status, parent or caregiver status, pregnant or postpartum status, and more.
- Starting October 2028, members earning above a certain income level will be asked to pay co-payments (specified dollar amounts that must be paid to a provider). Most routine services will be exempted, as will services delivered by certain safety net providers.
- HCPF estimates this will impact roughly 60,000 current members.
The new law also shifts massive financial costs from the federal government to the states. Colorado will be required to make significant changes to the way the state finances the state share of Medicaid costs. This will require difficult cost-shifting and cost-cutting measures within the state budget.
Yes. This bill affects SNAP eligibility and funding, although the federal government has yet to issue guidance on how and when changes will be implemented. Changes are not anticipated until at least October 2025.
Medicaid members should take extra care to keep their contact information up to date. Colorado Access, the state, and other partners will be in communication regarding upcoming changes that may affect members. The new law will require more frequent requests for information from many Health First Colorado members.
Rep. Joe Neguse (D)
2nd District:
Steamboat Springs, Vail, Boulder, Longmont, Fort Collins
DC office: 202-225-2161
Western Slope Office: 303-335-1045
Fort Collins Office: 970-372-3971
Boulder Office: 303-335-1045
Rep. Jeff Hurd (R)
3rd District:
Grand Junction, Pueblo, Durango, Gunnison, Craig
DC Office: 202-225-4676
Grand Junction Office: 970-208-0455
Pueblo Office: 719-696-6968
Durango Office: 970-317-6167
Rep. Lauren Boebert (R)
4th District:
Fort Morgan, Sterling, Limon, Lamar, Springfield, Lone Tree, Parker
DC Office: 202-225-4761
Lone Tree Office: 720-639-9165
Eaton Office: 970-702-2136
Rep. Jeff Crank (R)
5th District:
Colorado Springs
DC Office: 202-225-4422
Colorado Springs Office: 719-520-0055
Rep. Jason Crow (D)
6th District:
Aurora, Littleton
DC Office: 202-225-7882
Aurora Office: 720-748-7514
Rep. Brittany Pettersen (D)
7th District:
Arvada, Lakewood, Salida, Broomfield, Cañon City
DC Office: 202-225-2645
Lakewood Office: 303-274-7944
Cañon City Office: 719-458-6161
Rep. Gabe Evans (R)
8th District:
Greeley, Brighton, Thornton, Northglenn, Commerce City
DC Office: 202-225-5625
Northglenn Office: 303-723-6560
Greeley Office: 970-324-2567
Senator Michael Bennet (D)
DC office: 202-224-5852
Local office numbers:
Colorado Springs, CO: 719-328-1100
Denver, CO: 303-455-7600
Fort Collins, CO: 970-224-2200
Grand Junction, CO: 970-241-6631
Pueblo, CO: 719-542-7550
Alamosa, CO: 719-587-0096
Durango, CO: 970-259-1710
Senator John Hickenlooper (D)
DC office: 202-224-5941
Local office numbers:
Denver, CO: 303-244-1628
Colorado Springs, CO: 719-632-6706
Grand Junction, CO: 970-822-4530
Durango, CO: 970-880-7236
Greeley, CO: 970-352-5546
Fort Collins, CO: 970-484-3502
Glenwood Springs, CO: 970-989-7075
Get Involved
Join others who are getting their voices heard on social media by downloading the template, filling it out, taking your photo holding it, and sharing on all your social media channels. Make sure to tag us and use #MedicaidMatters and #MedicaidAwareness
Download the template here.

Who We Are
We are the largest and most experienced public sector health plan in the state, a nonprofit organization that goes beyond simply navigating health services. For over 30 years, we have transformed Colorado’s health care landscape through Health First Colorado, CHP+, physical and behavioral health, and the Colorado Access Foundation. As the state’s largest Medicaid plan with decades of experience, we felt it was crucial to speak up for millions of Medicaid members, providers, and partners during this confusing time. We hope this information helps clarify the current uncertainty and serves as a valuable resource.